By Josh Katz, Denise Lu
and Margot Sanger-Katz
April 28, 2020
https://www.nytimes.com/interactive/2020/04/28/us/coronavirus-death-toll-total.html
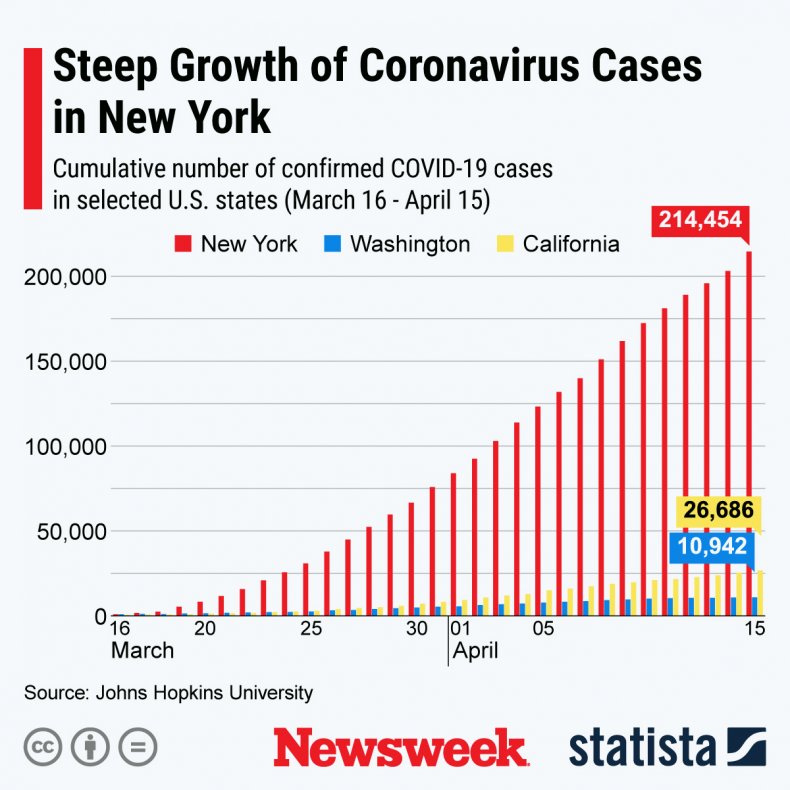
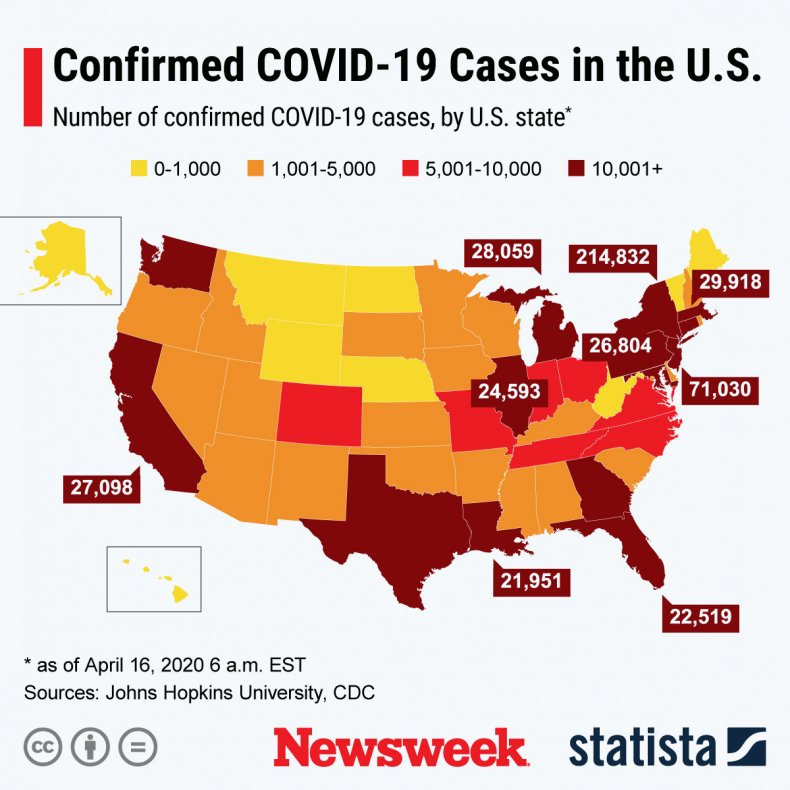
Total deaths in seven states that have been hard hit by the coronavirus pandemic are nearly 50 percent higher than normal for the five weeks from March 8 through April 11, according to new death statistics from the Centers for Disease Control and Prevention. That is 9,000 more deaths than were reported as of April 11 in official counts of deaths from the coronavirus.
The new data is partial and most likely undercounts the recent death toll significantly. But it still illustrates how the coronavirus is causing a surge in deaths in the places it has struck, probably killing more people than the reported statistics capture. These increases belie arguments that the virus is only killing people who would have died anyway from other causes. Instead, the virus has brought a pattern of deaths unlike anything seen in recent years.
If you look at the provisional deaths from all causes, death counts in New York, New Jersey, Michigan, Massachusetts, Illinois, Maryland and Colorado have spiked far above their normal levels for the period. In New York City, the home of the biggest outbreak, the number of deaths over this period is more than three times the normal number. (Recent data suggests it could have reached six times higher than normal.)
How reported coronavirus deaths compare with deaths above normal
Numbers are from March 8 to April 11, 2020.
AREA PCT. OF NORMAL EXCESS DEATHS−REPORTED COVID-19 DEATHS=GAP
New York City 325% 11,900 − 10,261 = 1,700
New Jersey 172% 5,200 − 2,183 = 3,000
New York (excluding N.Y.C.) 142% 4,200 − 2,425 = 1,700
Michigan 121% 2,000 − 1,391 = 600
Illinois 113% 1,400 − 682 = 700
Massachusetts 120% 1,200 − 686 = 500
Maryland 115% 700 − 207 = 500
Colorado 116% 600 − 274 = 300
In New Jersey, deaths have been 172 percent of the normal number so far — more than 5,000 additional deaths, compared with an average count from the past five years. In Michigan, the partial death count is 121 percent of the count in a normal year, the equivalent of nearly 2,000 more deaths.
These numbers are preliminary because death certificates take time to be processed and collected, and complete death tallies from the Centers for Disease Control and Prevention can take up to eight weeks to become final. The speed of that data reporting varies considerably by state. In Connecticut, for example, where reported coronavirus deaths are high, the C.D.C. statistics include zero reported deaths from any cause since Feb. 1, because of reporting lags.
We compared these provisional death counts with the average number of deaths each week over the past five years. Public health researchers use the term “excess deaths” to describe a gap between recent trends and a typical level of deaths.
It’s difficult to know whether the differences between excess deaths and the official counts of coronavirus deaths reflect an undercounting of coronavirus deaths or a surge in deaths from other causes. It’s likely a mix of both.
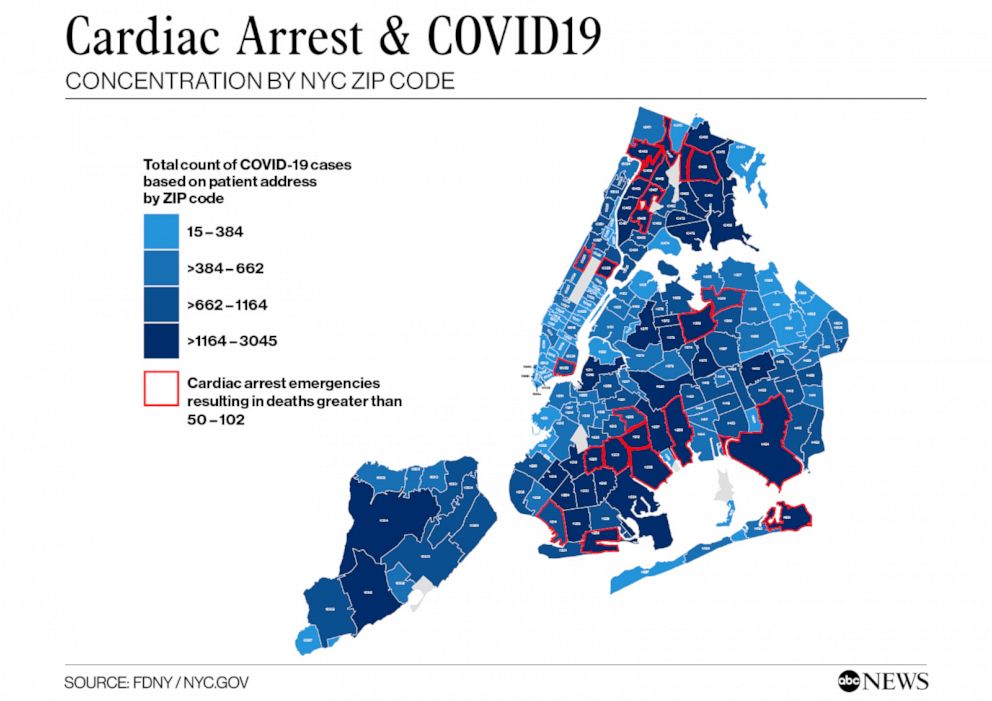
There is evidence, in New York and other places, that the official coronavirus counts are probably too low. Tests for the illness can be hard to get, and not all who die now are being tested, particularly if they die outside a hospital. New York City recently revised its own statistics for the number of coronavirus-related fatalities, saying thousands of additional deaths were probably because of Covid-19, even though no tests had been conducted.
There is also increasing evidence that stresses on the health care system and fears about catching the disease have caused some Americans to die from ailments that are typically treatable. A recent draft paper found that hospital admissions for a major type of heart attack fell by 38 percent in nine major U.S. hospitals in March. In a normal year, cardiovascular disease is the country’s leading cause of death.
Some causes of death may actually be going down. There appear to be fewer road fatalities in California, as more U.S. residents stay at home, for example. It is possible that those reductions could cancel out coronavirus deaths in places where the virus is not yet widespread. But, in many states, any such reductions have been clearly outweighed by increases in deaths directly and indirectly related to the virus.
Demographers often use measures of total deaths, sometimes called all-cause mortality, to evaluate the effects of natural disasters, where it can be difficult to trace particular causes.
In Puerto Rico in 2017, only 64 deaths were initially attributed to Hurricane Maria. But an analysis of the additional deaths showed the way that the disaster had, directly and indirectly, led to nearly 3,000 deaths over six months. The total included the immediate deaths from mudslides and drownings, but also sepsis, diabetes and suicides that came later as the power failure stretched on for months.
Coronavirus is clearly killing more U.S. residents directly than any hurricane has, but it is also changing lives in ways that may also contribute indirectly to increased deaths — by overloading the health care system and discouraging people from seeking care.
Measures of total deaths are also commonly used in countries without detailed accounting of causes of death. Right now, they are the most useful tool, several epidemiologists said, for measuring the impact of coronavirus in the United States, too.
“It gives you an overall sense of how big things are,” said Samuel Clark, a professor of sociology at Ohio State University, whose work is in demography and epidemiology. “For now, you can basically attribute the excess mortality to Covid-19. But you also grab all the things that are not Covid at all, but are probably created by the situation.”
Around the world, the coronavirus is bringing large waves of mortality. In Spain, deaths over the last month are 66 percent higher than normal, according to New York Times reporting. In Ecuador, they are more than 80 percent higher than normal. In Paris, more than twice as many people are dying every day as normal — far more than during a typical bad flu season.
Eventually, we will get more clarity about all of the reasons that people died this year. While no mortality statistics are ever perfect, the Centers for Disease Control and Prevention uses detailed death certificates to code the causes of death for everyone who dies each year in the United States. But that process typically takes more than a year to complete.
For now, total deaths are our best glimpse into the ways the coronavirus is affecting the normal patterns of survival.
New Jersey 172% 5,200 − 2,183 = 3,000
New York (excluding N.Y.C.) 142% 4,200 − 2,425 = 1,700
Michigan 121% 2,000 − 1,391 = 600
Illinois 113% 1,400 − 682 = 700
Massachusetts 120% 1,200 − 686 = 500
Maryland 115% 700 − 207 = 500
Colorado 116% 600 − 274 = 300
In New Jersey, deaths have been 172 percent of the normal number so far — more than 5,000 additional deaths, compared with an average count from the past five years. In Michigan, the partial death count is 121 percent of the count in a normal year, the equivalent of nearly 2,000 more deaths.
These numbers are preliminary because death certificates take time to be processed and collected, and complete death tallies from the Centers for Disease Control and Prevention can take up to eight weeks to become final. The speed of that data reporting varies considerably by state. In Connecticut, for example, where reported coronavirus deaths are high, the C.D.C. statistics include zero reported deaths from any cause since Feb. 1, because of reporting lags.
We compared these provisional death counts with the average number of deaths each week over the past five years. Public health researchers use the term “excess deaths” to describe a gap between recent trends and a typical level of deaths.
It’s difficult to know whether the differences between excess deaths and the official counts of coronavirus deaths reflect an undercounting of coronavirus deaths or a surge in deaths from other causes. It’s likely a mix of both.
There is evidence, in New York and other places, that the official coronavirus counts are probably too low. Tests for the illness can be hard to get, and not all who die now are being tested, particularly if they die outside a hospital. New York City recently revised its own statistics for the number of coronavirus-related fatalities, saying thousands of additional deaths were probably because of Covid-19, even though no tests had been conducted.
There is also increasing evidence that stresses on the health care system and fears about catching the disease have caused some Americans to die from ailments that are typically treatable. A recent draft paper found that hospital admissions for a major type of heart attack fell by 38 percent in nine major U.S. hospitals in March. In a normal year, cardiovascular disease is the country’s leading cause of death.
Some causes of death may actually be going down. There appear to be fewer road fatalities in California, as more U.S. residents stay at home, for example. It is possible that those reductions could cancel out coronavirus deaths in places where the virus is not yet widespread. But, in many states, any such reductions have been clearly outweighed by increases in deaths directly and indirectly related to the virus.
Demographers often use measures of total deaths, sometimes called all-cause mortality, to evaluate the effects of natural disasters, where it can be difficult to trace particular causes.
In Puerto Rico in 2017, only 64 deaths were initially attributed to Hurricane Maria. But an analysis of the additional deaths showed the way that the disaster had, directly and indirectly, led to nearly 3,000 deaths over six months. The total included the immediate deaths from mudslides and drownings, but also sepsis, diabetes and suicides that came later as the power failure stretched on for months.
Coronavirus is clearly killing more U.S. residents directly than any hurricane has, but it is also changing lives in ways that may also contribute indirectly to increased deaths — by overloading the health care system and discouraging people from seeking care.
Measures of total deaths are also commonly used in countries without detailed accounting of causes of death. Right now, they are the most useful tool, several epidemiologists said, for measuring the impact of coronavirus in the United States, too.
“It gives you an overall sense of how big things are,” said Samuel Clark, a professor of sociology at Ohio State University, whose work is in demography and epidemiology. “For now, you can basically attribute the excess mortality to Covid-19. But you also grab all the things that are not Covid at all, but are probably created by the situation.”
Around the world, the coronavirus is bringing large waves of mortality. In Spain, deaths over the last month are 66 percent higher than normal, according to New York Times reporting. In Ecuador, they are more than 80 percent higher than normal. In Paris, more than twice as many people are dying every day as normal — far more than during a typical bad flu season.
Eventually, we will get more clarity about all of the reasons that people died this year. While no mortality statistics are ever perfect, the Centers for Disease Control and Prevention uses detailed death certificates to code the causes of death for everyone who dies each year in the United States. But that process typically takes more than a year to complete.
For now, total deaths are our best glimpse into the ways the coronavirus is affecting the normal patterns of survival.