skip to main |
skip to sidebar
https://theconversation.com/deaths-and-desperation-mount-in-ecuador-epicenter-of-coronavirus-pandemic-in-latin-america-137015
Dead bodies are lying at home and in the streets of Guayaquil, Ecuador, a city so hard-hit by coronavirus that overfilled hospitals are turning away even very ill patients and funeral homes are unavailable for burial.
Data on deaths and infections is incomplete in Ecuador, as it is across the region. As of April 22, Ecuador – a country of 17 million people – had reported almost 11,000 cases, which on a per capita basis would put it behind only Panama in Latin America. But the true number is likely much higher.
The government of Guayas Province, where Guayaquil is located, says 6,700 residents died in the first half of April, as compared to 1,000 in a normal year. A New York Times analysis estimates Ecuador’s real coronavirus death toll may be 15 times the 503 deaths officially tallied by April 15.
In a pandemic that has largely hit wealthy countries first, Ecuador is one of the first developing countries to face such a dire outbreak.
Wealth is no guarantee of safety in an epidemic. Italy and the United States have both run short of necessary medical equipment like ventilators and dialysis machines. But experts agree poorer countries are likely to see death rates escalate quickly.
Our own academic research on Ecuadorean politics and human security in past pandemics suggests that coronavirus may create greater political and economic turmoil in a country that already struggles with instability.
Ecuador’s swift response
The coronavirus outbreak in Guayaquil, Ecuador’s largest city and economic engine, began in February, apparently with infected people returning from Spain.
 A doctor checking for COVID-19 symptoms in a family in Guayaquil, Ecuador, April 14, 2020. José Sanchez/AFP via Getty Images
A doctor checking for COVID-19 symptoms in a family in Guayaquil, Ecuador, April 14, 2020. José Sanchez/AFP via Getty Images
Its rapid escalation prompted panicked officials to impose social isolation quickly as a containment strategy. Ecuador’s restrictions on movement are strict and getting stricter.
Ecuadorians may not leave their homes at all between the hours of 2 p.m. and 5 a.m. Outside of curfew, they may only go out to get food, for essential work or for health-related reasons, wearing masks and gloves. Public transport is canceled.
In Quito, Ecuador’s capital, people may only drive one day a week as determined by their license plate.
This is the second time in a year Quito residents have found themselves under lockdown. In October 2019, a nighttime curfew was established quell massive protests against austerity measures that were imposed in exchange for a large loan from the International Monetary Fund.
The protests, led by indigenous groups, dissipated after President Lenín Moreno backed away from austerity – but not before at least eight people were killed.
Latin America’s looming epidemic
Ecuador has been more proactive in responding to the epidemic than many neighboring countries.
In Brazil President Jair Bolsonaro has largely downplayed the severity of the coronavirus, despite thousands of new COVID-19 infections reported every day. In Venezuela the power struggle between the government of Nicolás Maduro and the opposition government of Juan Guaidó impedes any coordinated pandemic response.
Most Latin American leaders who have taken decisive action against coronavirus see stay-at-home orders as the only way to avoid collapse of their fragile, underfunded health systems.
Panama is limiting outings based on gender, allowing men and women to leave their homes three days each. Everyone stays home on Sundays.
El Salvador’s president sent soldiers to enforce a 48-hour full lockdown of the city of La Libertad that prohibited residents from leaving home for any reason – including to get food or medicine.
It’s unclear how such restrictions can persist in a region with considerable poverty and social inequality. Large numbers of Latin Americans live day-to-day on money they make from street trading and other informal work, which is now largely banned. Hunger threatens across the region.
Fear-mongering over the deficit is the absolute wrong approach to the Covid-19 crisis.
BY JOSH BIVENS
https://inthesetimes.com/article/22494/debt-deficit-stimulus-recovery-mcconnell-covid-19
As policymakers scramble to try to mitigate the economic fallout of the coronavirus shock, a predictable chorus has emerged worrying that these efforts will lead to damaging increases in the nation’s public debt. The Washington Post and New York Times have been among the outlets sounding alarms over the implications of increased government spending. And even Senate Majority Leader Mitch McConnell (R-Ky.) warned against further economic stimulus, saying: “given the extraordinary numbers that we’re racking up to the national debt … we need to be as cautious as we can be.”
Baseless fears about deficits and debt were a prime impediment to doing the smart things for spurring a fast recovery from the Great Recession following the 2008 crash, and the result was a recovery that was far weaker than it should have been.
Before we repeat the same mistake this time, we should remember two important things about federal budget deficits and public debt. First, taking on debt can be stupid or smart—it depends on context, and the debt to GDP ratio provides no such context. Second, the popular analogy between household budgets and the budget of the federal government is actively misleading.
Let’s talk first about the difference between smart and dumb additions to debt. For a household, borrowing to go gamble at the racetrack would be dumb. But borrowing to finance an education that provided you with a skill or credential to increase your lifetime earnings would be smart—even if it’s a shame we make students take on debt at all.
For the federal government, deciding to add $1.5 trillion to the debt to give corporations tax cuts back in 2017 was dumb. But in the current crisis, taking on debt to finance expansions to unemployment insurance and aid to state and local governments and investments in hospitals and testing is very smart.
So, the threshold question for deciding whether or not to add to debt should simply be: is this dumb or is it smart—does it solve a pressing social problem or not? Debt used to finance relief and recovery measures is smart.
The second thing to keep in mind is that rules that apply to households about debt don’t apply to the U.S. government. People often claim that because households reduce spending during tough times as a precautionary measure, the federal government should too. But this is a terrible analogy, because what might make sense for one household to do in the face of anxiety about the economy leads to a crisis if everybody does it. In fact, the federal government should take on more debt exactly when households are trying to take on less.
Recessions start and worsen when it’s not just one household deciding to pull back spending, but millions of households. This is because one person’s spending is another person’s income. If I decide to delay buying a new washing machine because I’m worried about the economy, this reduces the incomes of the people making and selling washing machines. If those people in turn now have to pull back their spending because I didn’t buy anything from them…you can see the vicious cycle that can start and make recessions so damaging.
As private households start pulling back spending, and as this sets off a chain reaction that worsens a recession, you need some entity in the economy to break the downward spiral by ramping up its spending as private households ramp theirs down. That’s the federal government.
Further, this spending ramp-up should be financed by debt, not higher taxes that might drag on private spending. Even better than financing with debt might be printing money—but the distinction between debt and money-printing is a lot less important than the distinction between either of those and taxes.
Don’t get me wrong, we should raise taxes substantially and in a progressive way over the long-run to build a fairer and better economy. But we don’t need to do that before properly responding to the crisis in front of us.
An effective response in the next round of stimulus should include $500 billion in aid to state and local governments, make additional investments in unemployment compensation, protect workers’ paychecks, include worker protections and invest in our democracy. Yes, these actions will increase the debt, but they’re also critical to ensuring a real and fair recovery.
Some would say that allowing the debt to GDP ratio to climb back to levels last seen in the 1940s is a radical thing to do. It’s not—it’s just smart economics. But allowing unemployment and suffering to climb back to levels last seen in the 1930s while doing none of things we now know could avert that would be truly radical.
Ute Lotz-Heumann
https://theconversation.com/diary-of-samuel-pepys-shows-how-life-under-the-bubonic-plague-mirrored-todays-pandemic-136222
In early April, writer Jen Miller urged New York Times readers to start a coronavirus diary.
“Who knows,” she wrote, “maybe one day your diary will provide a valuable window into this period.”
During a different pandemic, one 17th-century British naval administrator named Samuel Pepys did just that. He fastidiously kept a diary from 1660 to 1669 – a period of time that included a severe outbreak of the bubonic plague in London. Epidemics have always haunted humans, but rarely do we get such a detailed glimpse into one person’s life during a crisis from so long ago.
There were no Zoom meetings, drive-through testing or ventilators in 17th-century London. But Pepys’ diary reveals that there were some striking resemblances in how people responded to the pandemic.
A creeping sense of crisis
For Pepys and the inhabitants of London, there was no way of knowing whether an outbreak of the plague that occurred in the parish of St. Giles, a poor area outside the city walls, in late 1664 and early 1665 would become an epidemic.
The plague first entered Pepys’ consciousness enough to warrant a diary entry on April 30, 1665: “Great fears of the Sickenesse here in the City,” he wrote, “it being said that two or three houses are already shut up. God preserve us all.”
Portrait of Samuel Pepys by John Hayls (1666). National Portrait Gallery
Pepys continued to live his life normally until the beginning of June, when, for the first time, he saw houses “shut up” – the term his contemporaries used for quarantine – with his own eyes, “marked with a red cross upon the doors, and ‘Lord have mercy upon us’ writ there.” After this, Pepys became increasingly troubled by the outbreak.
He soon observed corpses being taken to their burial in the streets, and a number of his acquaintances died, including his own physician.
By mid-August, he had drawn up his will, writing, “that I shall be in much better state of soul, I hope, if it should please the Lord to call me away this sickly time.” Later that month, he wrote of deserted streets; the pedestrians he encountered were “walking like people that had taken leave of the world.”
Tracking mortality counts
In London, the Company of Parish Clerks printed “bills of mortality,” the weekly tallies of burials.
Because these lists noted London’s burials – not deaths – they undoubtedly undercounted the dead. Just as we follow these numbers closely today, Pepys documented the growing number of plague victims in his diary.
At the end of August, he cited the bill of mortality as having recorded 6,102 victims of the plague, but feared “that the true number of the dead this week is near 10,000,” mostly because the victims among the urban poor weren’t counted. A week later, he noted the official number of 6,978 in one week, “a most dreadfull Number.”
By mid-September, all attempts to control the plague were failing. Quarantines were not being enforced, and people gathered in places like the Royal Exchange. Social distancing, in short, was not happening.
He was equally alarmed by people attending funerals in spite of official orders. Although plague victims were supposed to be interred at night, this system broke down as well, and Pepys griped that burials were taking place “in broad daylight.”
Desperate for remedies
There are few known effective treatment options for COVID-19. Medical and scientific research need time, but people hit hard by the virus are willing to try anything. Fraudulent treatments, from teas and colloidal silver, to cognac and cow urine, have been floated.
Although Pepys lived during the Scientific Revolution, nobody in the 17th century knew that the Yersinia pestis bacterium carried by fleas caused the plague. Instead, the era’s scientists theorized that the plague was spreading through miasma, or “bad air” created by rotting organic matter and identifiable by its foul smell. Some of the most popular measures to combat the plague involved purifying the air by smoking tobacco or by holding herbs and spices in front of one’s nose.
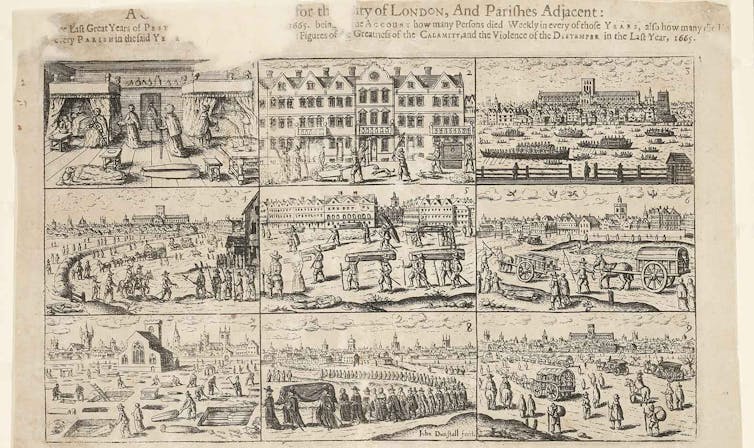
Tobacco was the first remedy that Pepys sought during the plague outbreak. In early June, seeing shut-up houses “put me into an ill conception of myself and my smell, so that I was forced to buy some roll-tobacco to smell … and chaw.” Later, in July, a noble patroness gave him “a bottle of plague-water” – a medicine made from various herbs. But he wasn’t sure whether any of this was effective. Having participated in a coffeehouse discussion about “the plague growing upon us in this town and remedies against it,” he could only conclude that “some saying one thing, some another.”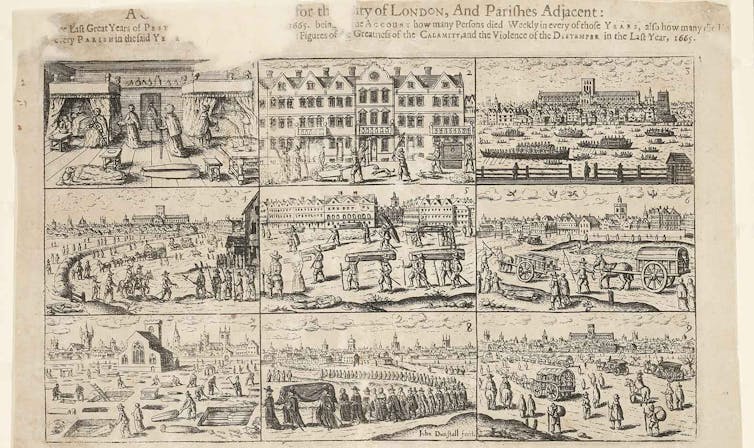 A 1666 engraving by John Dunstall depicts deaths and burials in London during the bubonic plague. Museum of London
A 1666 engraving by John Dunstall depicts deaths and burials in London during the bubonic plague. Museum of London
During the outbreak, Pepys was also very concerned with his frame of mind; he constantly mentioned that he was trying to be in good spirits. This was not only an attempt to “not let it get to him” – as we might say today – but also informed by the medical theory of the era, which claimed that an imbalance of the so-called humors in the body – blood, black bile, yellow bile and phlegm – led to disease.
Melancholy – which, according to doctors, resulted from an excess of black bile – could be dangerous to one’s health, so Pepys sought to suppress negative emotions; on Sept. 14, for example, he wrote that hearing about dead friends and acquaintances “doth put me into great apprehensions of melancholy. … But I put off the thoughts of sadness as much as I can.”
Balancing paranoia and risk
Humans are social animals and thrive on interaction, so it’s no surprise that so many have found social distancing during the coronavirus pandemic challenging. It can require constant risk assessment: How close is too close? How can we avoid infection and keep our loved ones safe, while also staying sane? What should we do when someone in our house develops a cough?
During the plague, this sort of paranoia also abounded. Pepys found that when he left London and entered other towns, the townspeople became visibly nervous about visitors.
“They are afeared of us that come to them,” he wrote in mid-July, “insomuch that I am troubled at it.”
Pepys succumbed to paranoia himself: In late July, his servant Will suddenly developed a headache. Fearing that his entire house would be shut up if a servant came down with the plague, Pepys mobilized all his other servants to get Will out of the house as quickly as possible. It turned out that Will didn’t have the plague, and he returned the next day.
In early September, Pepys refrained from wearing a wig he bought in an area of London that was a hotspot of the disease, and he wondered whether other people would also fear wearing wigs because they could potentially be made of the hair of plague victims.
And yet he was willing to risk his health to meet certain needs; by early October, he visited his mistress without any regard for the danger: “round about and next door on every side is the plague, but I did not value it but there did what I could con ella.”
Just as people around the world eagerly wait for a falling death toll as a sign of the pandemic letting up, so did Pepys derive hope – and perhaps the impetus to see his mistress – from the first decline in deaths in mid-September. A week later, he noted a substantial decline of more than 1,800.
Let’s hope that, like Pepys, we’ll soon see some light at the end of the tunnel.
Where we are now
Researchers have begun to publish studies about coronavirus antibodies, and our ace health care reporter Caroline Chen breaks down what these studies can tell us — and more importantly, what they can’t. Even a test that is very good can give out more false positives than true positives when the prevalence of a disease is very low in a population.
My ProPublica Illinois colleague Haru Coryne looked at how coronavirus has spread in Chicago. His analysis found that crowded conditions within homes, rather than housing density, may better explain why some areas of the city see higher infection rates.
Taken together, these two stories help us understand how the coronavirus is spreading and how we can find a path forward.
Holding companies accountable
At a time when much of the retail sector is collapsing, Amazon is strengthening its competitive position in ways that could outlast the pandemic — and raise antitrust concerns, Renee Dudley reported.
One thing that hasn’t fully stopped during the pandemic: Aggressive medical-debt collection. U.S. hospitals are in the spotlight for being on the front line of fighting COVID-19. But Alec MacGillis found that in the shadows, debt collection operations continue, often by the same institutions treating coronavirus patients.
Meanwhile at health insurance giant Cigna, executives told analysts the pandemic wouldn’t hurt its business, but a trade group that represents Cigna and other insurers asked Congress for aid.
Holding government accountable
FEMA has helped pay for the burials of victims of past disasters. But months into the coronavirus pandemic, the Trump administration has sat on similar requests. Families of COVID-19 victims have been forced to turn to religious centers and GoFundMe. So far, approximately 30 states and territories have requested the funding.
Sen. Richard Burr, who is under investigation for his stock trading, is not just a friend to the health care industry. He’s also a stockholder. He regularly flips health care stocks even as he pushes for legislation to help the industry. Burr has denied doing anything improper.
All vote by mail systems are not created equal, Ryan McCarthy reported, and whether the ballot you mail is counted may depend on where you vote. Disputes between policymakers in at least six states cast doubt about whether states can make a smooth and equitable shift from in-person to mail-in ballots by November.
https://www.iflscience.com/health-and-medicine/can-you-get-covid19-from-delivery-food/
As one-third of humanity is cooped up in their homes and people are forced to eat their own cooking, food delivery services are seeing increased sales during the COVID-19 pandemic.
Like other coronaviruses, SARS-CoV-2 is thought to mainly spread from person-to-person through respiratory droplets that are expelled from an infected person when they cough, sneeze, or talk. People can become infected with the virus through close contact with an infected individual or through touching contaminated surfaces and then touching their face, according to the Centers for Disease Control and Prevention (CDC).
But can takeout also serve as a vector?
To date, there is no evidence that SARS-CoV-2, the virus that causes COVID-19, can be transmitted through eating food. However, there is a possible risk that the virus may persist on food packaging like plastic for up to 72 hours, according to a study published last month in the New England Journal of Medicine. On cardboard, researchers found no viable evidence of the virus after 24 hours. On all surfaces, the virus degrades quickly and is seen to drop by half within just under seven hours on plastic and within about three hours on cardboard.
“There are two important messages on handling food and food safety at this time. One is about preventing COVID-19 spread and shopping for food and the other is about keeping your food safe and preventing food poisoning at home,” said Cathy Moir, council chair for the Food Safety Information Council, in a statement.
COVID-19 is not considered a foodborne illness and it is not believed to be transmitted through food. However, there is a risk that SARS-CoV-2 can be transmitted by surface cross-contamination. There are varying reports of how long COVID-19 can remain on surfaces. The World Health Organization, for example, says that it is not certain how long the virus can last on a surface, but based on its behavior similar to other coronaviruses, it may persist for a few hours or up to several days, though that timeframe may vary under different environmental conditions and the type of surface. One report found that the virus persisted on cruise ship surfaces for up to 17 days.
“Currently there is no evidence of food or food packaging being associated with the transmission of COVID-19. Like other viruses, it is possible that the virus that causes COVID-19 can survive on surfaces or objects. For that reason, it is critical to follow the 4 key steps of food safety – clean, separate, cook, and chill,” writes the US Department of Agriculture. The agency adds that there is also no evidence to suggest that food produced within the country can transmit COVID-19, nor can goods that are imported from other nations.
When home from shopping or after grabbing takeout, the Institute for Food Safety says that individuals should first place shopping bags on the floor and immediately wash their hands. Discard or recycle any single-use bags. Wash your hands but keep in mind that there is no need to discard or sanitize any part of the actual food packaging. Best practices follow that fruits and vegetables should be rinsed and foods with a hard surface, like apples or carrots, should be scrubbed. “NEVER” use soap or bleach as these may have negative health impacts if left on food and accidentally consumed. The institute adds that the coronavirus is killed by “cooking to the safe minimum cooking temperatures specified by the FDA and USDA.”
When it comes to cooking, the US Food and Drug Administration (FDA) reminds consumers that foodborne gastrointestinal viruses, like norovirus and hepatitis A, can still make people ill through contaminated food. People preparing to stay home for extended periods of time need to practice basic food safety and hygiene measures, like washing hands and surfaces often, separating raw meat from other foods, cooking to the right temperature, and refrigerating foods, according to a tipsheet provided by the USDA.
April 20, 2020
https://www.advisory.com/daily-briefing/2020/04/20/covid-count
CDC relies on state-by-state tallies of death certificates to calculate the number of U.S. deaths from the new coronavirus, but state officials warn that the process is riddled with inaccuracies—and experts say the number of Americans who've died from the virus is likely higher than CDC's official count.
Covid-19 weekly webinar: What you need to know in 45 minutes
US Covid-19 death toll tops 30K
As of Monday morning, U.S. officials had reported 753,317 cases of Covid-19, the disease caused by the new coronavirus and 36,109 U.S. deaths linked to the new coronavirus.
Covid-19 death count strategies vary between states
But health experts say inconsistent counting methods and a lengthy national data-gathering strategy likely mean the nationwide estimates of Covid-19 cases and deaths are inaccurate.
Until last week, CDC's national Covid-19 case and death counts only included cases and deaths that were confirmed with a laboratory test. However, CDC on Tuesday announced that it would begin including "probable [Covid-19] cases and deaths" in the totals because testing shortages hampered some states' ability to test every patient suspected of having Covid-19.
For instance, New York City—which is an epicenter of the United States' Covid-19 epidemic—this week began including presumed Covid-19 deaths in its count, which led to a significant spike in the number of Covid-19 deaths the city has reported. Officials said the additional deaths occurred among individuals who did not have lab tests confirming they were positive for the new coronavirus, but whose death certificates list Covid-19 as their suspected cause of death based on their medical histories and symptoms.
Delaware, Connecticut, Maryland, Ohio, and Pennsylvania also have started including probable cases and deaths in their reported tallies.
Other states have included probable cases and deaths in their tallies since they first began reporting the numbers, the Washington Post reports. Colorado, for instance, has included "epidemiologically linked" cases, or cases among people who were never tested for the new coronavirus but had contact with an infected person and showed symptoms of the disease, in its statewide death count since March. "Epidemiologically linked" cases accounted for about 3% of the state's Covid-19 death count as of Thursday.
In comparison, other states have unique counting strategies that can sometimes exclude even laboratory-confirmed cases of Covid-19 from their death tallies, the Post reports.
For example, in Alabama, a physician reviews the medical records of people who died and tested positive for Covid-19 to determine whether the death should be attributed to Covid-19 or to another underlying health condition. According to Karen Landers, a spokesperson for the state's Department of Public Health, Alabama's death count often excludes people who tested positive for Covid-19 but had no respiratory symptoms as well as people who experienced another health event, like a heart attack, when they had the disease.
As a result, out of the 110 people in Alabama who had tested positive for Covid-19 and died as of Thursday, 73 were included in the statewide death tally sent to CDC, the Post reports. Another 12 deaths were excluded, and 25 other deaths are still under review, according to the Post.
Deborah Birx, a physician who's leading the White House's coronavirus task force, said Alabama's strategy conflicts with CDC's approach to tallying Covid-19-realted deaths. "[W]e've taken a very liberal approach to mortality," she said. "[I]f someone dies with Covid-19, we are counting that as a Covid-19 death."
However, health experts said the nature of the disease, which can be mild and even asymptomatic in some, and the nation's testing hurdles inevitably will result in discrepancies in how Covid-19 cases and deaths are counted.
"Can there be disagreement in how these things are concluded? Absolutely," said Jonathan Arden, a forensic pathologist and chair of the board of the National Association of Medical Examiners. "You are talking about medical judgments, a diagnostic process that means you are arriving at an opinion."
Officials suspect underreporting of Covid-19
Meanwhile, city officials have told ProPublica that an increase in the rate of at-home deaths across the country could imply that the official U.S. Covid-19 death count is excluding a number of deaths that are occurring outside of hospitals.
ProPublica in a review compiled data from health agencies, police departments, 911 call centers, and vital-records departments to analyze overall death rates in states that house Covid-19 hot zones, including Massachusetts, Michigan, New York, and Washington. According to ProPublica, New York City officials last week recorded about 200 deaths per day that occurred outside of nursing homes and hospitals, compared with an average of about 35 such deaths per day between 2013 and 2017. Similarly, in Detroit, officials received more than 150 "dead person observed" phone calls within the first 10 days of April, compared with an average of about 40 during the same time period in recent years.
And in Middlesex County, Massachusetts, officials reported 317 at-home deaths in March this year, representing a 20% increase when compared with the number of at-home deaths reported during March in recent years, ProPublica found. The official Covid-19 death rate for the state was 89 in March, according to Massachusetts' Department of Public Health.
According to ProPublica, health experts have said the large increases in at-home deaths in these states could stem from deaths occurring among people who were infected with the new coronavirus, but who were not included in the states' overall Covid-19 death count due to a lack of access to treatment or testing.
However, some experts cautioned that the increases in at-home deaths in these states also could be tied to growth in the number of people dying at home from other conditions, such as heart attacks, because they either couldn't get to a hospital or were afraid to seek hospital care because of the Covid-19 epidemic.
'Just the tip of the iceberg'?
Still, Mark Hayward, a sociology professor at the University of Texas-Austin, said the discrepancies likely mean America's current official Covid-19 death count represents "just the tip of the iceberg" of how deadly the disease has been in country. "[T]he undercount is going to be really high" at the start of the epidemic, he said.
Robert Anderson, chief of CDC's mortality statistics branch, said national death counts based on death certificates always are an underestimate, even for common illnesses like the flu. Eventually, CDC likely will adjust its national death count for Covid-19 by comparing the total deaths recorded during the epidemic to historic death rates, Anderson said (Brown et al., Washington Post, 4/16; Bowden, The Hill, 4/16; Gillum, ProPublica, 4/14).
 A doctor checking for COVID-19 symptoms in a family in Guayaquil, Ecuador, April 14, 2020. José Sanchez/AFP via Getty Images
A doctor checking for COVID-19 symptoms in a family in Guayaquil, Ecuador, April 14, 2020. José Sanchez/AFP via Getty Images Colombians under mandatory quarantine hang red fabric out their windows to request food aid, Soacha, April 15, 2020. Leonardo Munoz/VIEWpress via Getty Images
Colombians under mandatory quarantine hang red fabric out their windows to request food aid, Soacha, April 15, 2020. Leonardo Munoz/VIEWpress via Getty Images Street vendors in Guayaquil, Ecuador, April 17, 2020. Eduardo Maquilón/Agencia Press South/Getty Images
Street vendors in Guayaquil, Ecuador, April 17, 2020. Eduardo Maquilón/Agencia Press South/Getty Images